Liver surgery (hepatectomies)
Indications
 Most hepatectomies are performed for the treatment of hepatic neoplasms, either benign or malignant. Benign neoplasms include hepatocellular adenoma, hepatic hemangioma, and focal nodular hyperplasia. The most common malignant neoplasms (cancers) of the liver are metastases; those resulting from colorectal cancer are among the most common and most likely to undergo surgical resection. The most common primary malignant liver tumor is hepatocellular carcinoma. Hepatectomy may also be the procedure of choice to treat intrahepatic gallstones or parasitic liver cysts. Partial hepatectomies are also performed to remove part of the liver from a living donor for transplantation.
Most hepatectomies are performed for the treatment of hepatic neoplasms, either benign or malignant. Benign neoplasms include hepatocellular adenoma, hepatic hemangioma, and focal nodular hyperplasia. The most common malignant neoplasms (cancers) of the liver are metastases; those resulting from colorectal cancer are among the most common and most likely to undergo surgical resection. The most common primary malignant liver tumor is hepatocellular carcinoma. Hepatectomy may also be the procedure of choice to treat intrahepatic gallstones or parasitic liver cysts. Partial hepatectomies are also performed to remove part of the liver from a living donor for transplantation.
Techniques
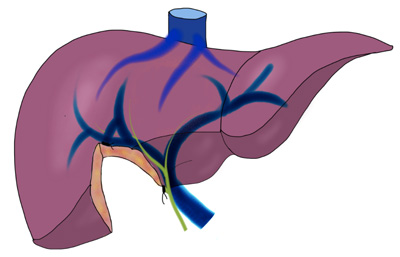
A hepatectomy is considered major surgery performed under general anesthesia. Access is achieved by laparotomy, usually through a bilateral subcostal ("chevron") incision, possibly with midline extension (Calne's incision). An earlier approach, one of the most innovative, is simplified by the liver suspension maneuver. Hepatectomies can be anatomical, that is, the lines of resection correspond to the limits of one or more functional segments of the liver as defined by Couinaud's classification; or they may be non-anatomic, irregular, or "wedge" hepatectomies. Anatomical resections are generally preferred due to the lower risk of bleeding and biliary fistula; however, non-anatomic resections can also be performed safely in some cases. The Pringle maneuver is usually performed during hepatectomy to minimize blood loss – however, this can lead to reperfusion injury to the liver due to ischemia
Complications
LHaemorrhage is the most feared technical complication and may justify urgent reoperation. Biliary fistula is also a possible complication, although it lends itself more to non-surgical management. Pulmonary complications such as atelectasis and pleural effusion are common and dangerous in patients with underlying lung disease. The infection is relatively rare.
Liver failure poses a significant risk to patients with underlying liver disease; it is a major deterrent in the surgical resection of hepatocellular carcinoma in patients with cirrhosis. It is also a problem, to a lesser extent, in patients who have had previous hepatectomies (eg, repeat resections for reincident colorectal cancer metastases).
Results
Liver surgery is safe when performed by experienced surgeons with appropriate technological and institutional support. As with most major surgeries, there is a marked trend toward optimal outcomes from surgeons with high workloads in selected centers (usually cancer centers and transplant centers)
For optimal results, combination therapy with chemotherapy or systemic or regional biological therapy should be considered. Prior to surgery, cytotoxic agents such as systemically administered oxaliplatin for colorectal metastases, or chemoembolization for hepatocellular carcinoma can significantly reduce the size of the tumor mass, allowing resections that would only remove a segment or a corner part of the liver. These procedures can also be facilitated by the application of a liver clamp to minimize blood loss
Operative follow-up after hepatectomy
The patient is directed to the intensive care unit where he will spend 48 hours on average. If he has not been awakened in the recovery room, he will gradually be in intensive care. He is carrying an infusion, a urinary catheter but the gastric tube is removed as soon as he wakes up. Blood pressure, pulse and other cardiovascular parameters are constantly monitored by electronic devices which retransmit the results on a screen.
The 2 main complications that can occur during the stay in intensive care are:
The haemorrhage which, if significant, will require a transfusion and/or reoperation.
Liver failure related to the volume of liver removed and the state of the liver before the procedure (existence of cirrhosis). This hepatic insufficiency is generally transient and not very serious unless it persists beyond the fifth day. If these risks are ruled out, the patient is transferred to the traditional hospitalization unit where he will stay for 8 to 10 days. The patient will eat again as soon as intestinal transit resumes, the urinary catheter will be quickly removed, the abdominal drain from the 4th day if it no longer gives anything. Monitoring will be clinical (temperature, blood pressure, examination of the scar) and biological (coagulation factors, liver enzymes, white and red blood cells).
Two specific complications can occur during this period:
Biliary fistula: bile flows through the drain (yellow liquid). If the flow is low, this fistula will dry up spontaneously. In case of high flow it signs a wound of a large bile duct. It is not necessary to re-operate the patient. These fistulas are treated endoscopically by slipping a plastic prosthesis into the main bile duct which will be removed once the fistula has dried up.
The collection on the section edge: it can be a hematoma or a bilious collection (we speak of bilioma) superinfected. Clinically the patient is febrile, sometimes embarrassed to breathe. The level of white blood cells in the blood is high and the liver biological test is disturbed. The scanner makes it possible to make the diagnosis and to treat this abscess by draining it percutaneously under local anesthesia.