In vitro fertilization
Definition
 In vitro fertilization ( IVF ) is a procedure developed by the Englishman Robert Edwards, thanks to which - in 1978 - Louise Brown was born, the fruit of her studies as well as the first human being conceived in a test tube.
In vitro fertilization ( IVF ) is a procedure developed by the Englishman Robert Edwards, thanks to which - in 1978 - Louise Brown was born, the fruit of her studies as well as the first human being conceived in a test tube.
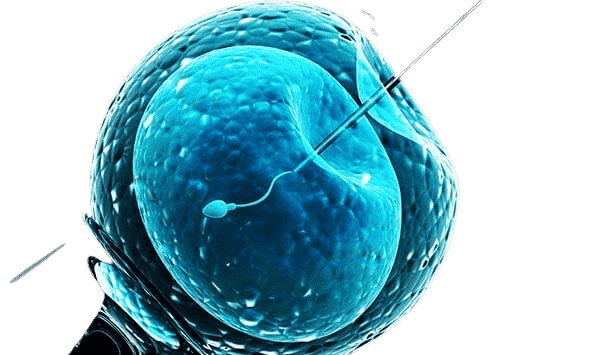
The technique is based on the retrieval of oocytes through the vagina and their subsequent fertilization in the laboratory, using the spermatozoa of the partner or of an anonymous donor. Likewise, if the female germ cells are unsuitable for generation, oocytes from a donor outside the couple can be used.
Once fertilization has taken place, one to three embryos are simultaneously transferred into the woman's uterus, the natural place of their development.
When to use?
In vitro fertilization is traditionally used in cases of alteration and obstruction of the tubes (tubal sterility) or their congenital or acquired absence (for example by surgical removal).
As seen in the article dedicated to female infertility, all these conditions prevent or make it very difficult for the egg to meet the sperm. The union of the gametes is then carried out in the laboratory by circumventing the organic impediment.
To also consider the possibility of giving a pregnancy to women whose ovaries have been removed, to those who lack them since birth and in all cases of ovarian failure. In the absence of this essential organ for female hormonal regulation, it is not only necessary to resort to oocytes donated by another woman, but also to guarantee the implantation and the course of the pregnancy by the association of hormone replacement therapy. appropriate .
The same technique can be used in the presence of endometriosis, low sperm viability, or when artificial insemination fails.
How it's made?
First, the woman's ovulation is controlled by hormonal stimulation, with the aim of producing multiple ovulation. The need to collect more oocytes stems from a simple consideration: the more embryos transferred to the uterus, the greater the chances of implantation.
Oocytes are collected under ultrasound guidance, most often under general anesthesia, selected and left to incubate at 37 degrees, for 24 to 48 hours, in prepared liquids and with a selected population of spermatozoa.
After this period, if fertilization has taken place, as happens in 70-90% of cases, the embryos are transferred to the uterus; in general, their number is chosen according to the woman's age: 1-2 if she is under 36, 2-4 in older women. Those that remain, called supernumeraries, are frozen and stored for years.
Embryo storage
The need to save these embryos stems from the fact that repeated ovarian stimulation operations, in addition to being costly in economic terms, can be dangerous for women's health. Seen from this angle, the freezing of embryos in liquid nitrogen (-196°C) represents a precious resource in the event of failure of the first attempts at birth.
In Italy, however, it is possible to produce no more than three embryos at a time, that is, the number necessary for a single and simultaneous implantation. An alternative to freezing embryos, prohibited in our country, could be to do the same with eggs. This possibility poses far fewer ethical problems; unfortunately, however, the biological characteristics of the egg make the operation quite delicate and it is still too early to assess whether freezing it is totally harmless for the health of the unborn child.
Chance of success
Of the 2 to 4 embryos transferred to the woman's uterus, at least one should be able to implant and thus establish the long-awaited pregnancy.
The number of embryos is then chosen by deciding between the possibility of failure and a possible multiple pregnancy.
This is an important choice because a multiple pregnancy could compromise the very outcome of the pregnancy and the health of the mother and fetus. On the other hand, the success rates of in vitro fertilization are not very high, so much so that it is on average 35% if the woman is under 36 years old, down to percentages below 9% for over 40 years. . In addition, the abortion rate is quite high, close to 20%, as is the risk of twin pregnancies. There also appears to be an increased likelihood of premature births and low birth weight babies.