Hysteroscopy
Definition
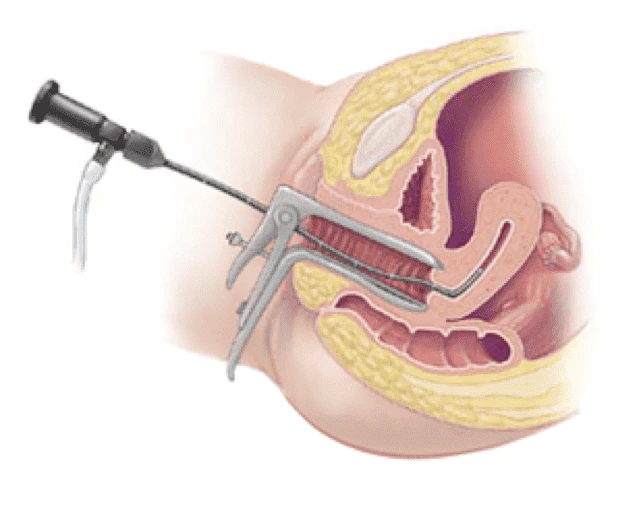 Hysteroscopy is an endoscopic gynecological intervention, which makes it possible to observe the uterus from the inside and possibly to set up a therapeutic action. Act performed on an outpatient basis, hysteroscopy can be used for the diagnosis of various pathologies of the uterus or it can have therapeutic aims. Hysteroscopy requires the patient to undergo preparatory tests, which essentially serve to avoid adverse effects and to ensure that there are no contraindications. From a procedural point of view, hysteroscopy is characterized by the insertion into the uterus, through the vaginal opening, of a probe-instrument, called a hysteroscope.
Hysteroscopy is an endoscopic gynecological intervention, which makes it possible to observe the uterus from the inside and possibly to set up a therapeutic action. Act performed on an outpatient basis, hysteroscopy can be used for the diagnosis of various pathologies of the uterus or it can have therapeutic aims. Hysteroscopy requires the patient to undergo preparatory tests, which essentially serve to avoid adverse effects and to ensure that there are no contraindications. From a procedural point of view, hysteroscopy is characterized by the insertion into the uterus, through the vaginal opening, of a probe-instrument, called a hysteroscope.
The duration of hysteroscopy varies from a minimum of 10 minutes to a maximum of approximately 60 minutes.
Hysteroscopy presents certain risks, more or less important; in general, however, the procedure takes place without particular problems.
How to prepare for a Hysteroscopy?
Hysteroscopy requires special preparation, as the procedure is not suitable for all women and, if it is for therapeutic purposes, it could include the use of general anesthesia.
Therefore, before a hysteroscopy can be performed, a gynecologist must first establish the suitability of the hypothetical patient for the procedure and, subsequently, provide all the indications relating to the behaviors to be adopted so that the whole protocol runs for the best.
In the case of a diagnostic hysteroscopy, a careful gynecological examination and an accurate assessment of the clinical history (anamnesis) are usually sufficient to establish a woman's suitability for the procedure; if the possibility of pregnancy or cervico-vaginal tract infection appears, a reliable pregnancy test or cervico-vaginal swab, respectively, is added to the above investigations.
In the case of an operative hysteroscopy, the following are necessary to determine a woman's suitability for the procedure:
Gynecological examination.
Clinical history assessment.
Blood tests and electrocardiogram (these are essential for general anesthesia).
Cervicovaginal swab (only in case of suspected genital infection).
Pregnancy test (only if you think you might be pregnant).
How to dress on the day of the procedure?
On the day of the procedure, gynecologists advise patients who are suitable for hysteroscopy to wear comfortable and practical clothing, as they will then be replaced in favor of a hospital gown specially prepared by the medical staff.
Hysteroscopy and general anesthesia
If the hysteroscopy involves general anesthesia, the patient must be fasting for at least 8 hours on the day of the operation; this means that, if the examination is scheduled for the morning, the last authorized meal is that of the day before.
Failure to fast will result in the intervention being postponed to another date.
It should be noted that in general the patient is allowed to drink water up to 2-3 hours before the general anesthesia.
Hysteroscopy and the menstrual cycle: when to do it?
For menstruating women, the best time to perform a hysteroscopy is within the first seven days after menstruation; in fact, performing the procedure at this time of the menstrual cycle allows gynecologists to get a better and more detailed view of the uterus and its internal cavities.
Procedure of the hysteroscopy
There are four strengths of hysteroscopy procedures:
The positioning of the patient and the placement of any anesthesia. This is the first moment.
The introduction of the hysteroscope into the uterus and the distention of the internal uterine walls. This is the phase that begins after the positioning of the patient and the possible implementation of anesthesia.
The internal exploration of the uterus and the possible removal of a tissue sample, in the case a diagnostic hysterectomy, or therapeutic intervention, in the case of an operative hysterectomy (*). This is the third step of the procedure.
The extraction of the hysteroscope. This is the last moment of the hysteroscopy.
NB: Please note that operative hysteroscopy can also be used to perform operations related to contraception (eg extraction of the intrauterine system; closure of the fallopian tubes).
Recovery
After a diagnostic hysteroscopy, the patient can resume her normal daily activities the day after the procedure; the only limitation foreseen concerns the sexual sphere: he must abstain from sexual intercourse for at least 1-2 weeks.
After an operative hysteroscopy, on the contrary, the patient must observe a few days of absolute rest; after which he can resume his normal daily activities, but very gradually.
Even in these situations, it is important to abstain from sexual activity for at least 7-14 days.
It should be noted that in the first 24 hours following the intervention, in the event that it involves general anesthesia, the patient may feel a slight feeling of confusion which gradually fades.
Risks and Complications
Hysteroscopy is associated with a risk of adverse effects and complications; however, in most cases it goes well or causes little or no discomfort, so the medical community considers it a safe procedure.By side effects, we mean minor, fairly frequent and temporary problems (maximum duration of 24 to 48 hours).Possible side effects associated with hysteroscopy are:
Light vaginal bleeding. It is the result of damage caused by passing the hysteroscope along the cervix and cervical canal.
Abdominal pain and cramps. Often the painful sensation can be controlled with a pain reliever, such as paracetamol or ibuprofen (an NSAID).
Feeling tired and/or ill.
Reflex pain in the shoulder, resulting from the use of gas rich in carbon dioxide.
Complications are defined as clinically relevant problems, which may arise during the procedure or at its conclusion and which require specific medical treatment.Possible complications associated with hysteroscopy are:
Uterine perforation.
Bladder perforation.
The development of pelvic infection (metritis).
Laceration of blood vessels in the uterus leading to heavy vaginal bleeding.
Endometritis, i.e. inflammation of the endometrium.
Peritonitis, i.e. inflammation of the peritoneum.
Severe allergic reaction (anaphylactic shock) to anesthetics.
Oedema in the uterus.
Air embolism (it is related to the practice of general anesthesia).
Cervical trauma caused by hysteroscope.
It should be noted that the risk of complications is very low: estimates report, in fact, that less than 1% of women undergoing hysteroscopy encounter one of the aforementioned complications.
Results
Hysteroscopy is a procedure that is increasingly used because it has several advantages:
It is effective, both when it has diagnostic aims and when it has therapeutic aims.
She is safe. As stated above, the risk of complications is low.
It is minimally invasive and painless.
This is usually not a reason for hospitalization. Unless there are serious complications, the patient can go home immediately after the operation or at the latest after a few hours.
In some situations it is a valid alternative to hysterectomy, laparoscopic surgery and laparotomy.
It usually takes a few weeks to know the results of a hysteroscopy with biopsy.