Meniscal lesions - meniscectomy - of the knee
Meniscal lesions
 Meniscus lesions are common and affect the entire population. They can be traumatic and/or degenerative. They cause joint pain, blockages and effusions. Their treatment is simple and consists of resection or suture performed under local joint anesthesia and outpatient surgery. Arthroscopic treatment allows a very rapid return to activities.
Meniscus lesions are common and affect the entire population. They can be traumatic and/or degenerative. They cause joint pain, blockages and effusions. Their treatment is simple and consists of resection or suture performed under local joint anesthesia and outpatient surgery. Arthroscopic treatment allows a very rapid return to activities.
What is a meniscal lesion?
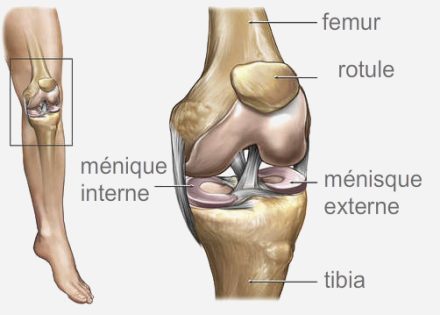
 There are 2 menisci in the knee, one on the inside (the internal meniscus), the other on the outside (the external meniscus). These menisci are crescent-shaped fibro-cartilages intercalated between femur and tibia. They act as stabilizing wedges for the knee and also harmoniously increase the joint contact surface. These meniscal lesions are of 2 types:
There are 2 menisci in the knee, one on the inside (the internal meniscus), the other on the outside (the external meniscus). These menisci are crescent-shaped fibro-cartilages intercalated between femur and tibia. They act as stabilizing wedges for the knee and also harmoniously increase the joint contact surface. These meniscal lesions are of 2 types:
Degenerative, i.e. related to wear and aging of the knee.
Traumatic, that is to say following a sprain or forced bending of the knee.
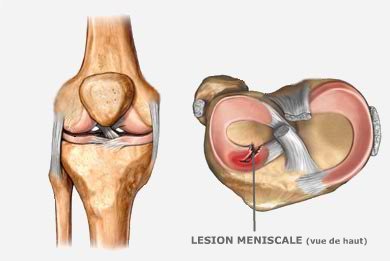
They more often reach the internal meniscus than the external meniscus. They are distinguished according to their location (anterior horn, middle part, posterior horn) and according to their type (vertical or oblique longitudinal fissure, radial or horizontal) .
Malformations are rare and are located almost exclusively on the external meniscus. It is anterior or posterior megacorn or discoid meniscus. These malformations are sometimes asymptomatic and therefore do not need to be operated on. Sometimes they cause pain and arthroscopic meniscoplasty is then performed. Meniscal cysts are sometimes present in association with a meniscal lesion. They occur more often on the outer meniscus than on the inner meniscus. They are often treated arthroscopically during meniscal regularization. An enlargement of their articular orifice is made so that the cyst can drain.
Why meniscal surgery or meniscectomy?
The tearing of a meniscus is painful, more rarely at the origin of blockages of the knee. When necessary, it is treated either by resection of the torn area or by repair by suture. Meniscectomy is performed arthroscopically. It is necessary to treat the meniscal lesion and avoid pain and blockages. It is also necessary to treat the possible consequences of this meniscal lesion which are:
The extension of the lesion and therefore a greater deterioration of the meniscal apparatus. Conservative surgery becomes less obvious and meniscal resection more important.
The appearance of cartilage lesions next to the meniscal lesion. They are generally due to repeated dislocations of the meniscal tongue. They are irreversible.
The appearance of a popliteal cyst due to recurrent effusions of synovial fluid and inflammatory condition chronicle of the knee.
What type of intervention?
Three treatment options are available to us:
Withholding treatment if the lesion is small and very peripheral or if it does not completely cross the meniscus and what occurs on a stable knee, ie without ligament damage.
Meniscal regularization which consists of essentially removing the meniscal lesion while trying to preserve as much of the meniscus as possible.
The meniscal suture which consists of repairing the meniscus using absorbable anchors or arrows. It is a totally conservative intervention.
These interventions are carried out under arthroscopy by 2 mini incisions of less than 5 mm through which a camera and the instruments are introduced which will make it possible to treat the meniscal lesion. The joint is then inflated with water, which allows constant washing and reduces the risk of infection. These procedures are performed on an outpatient basis
Risks and Compliactions
In addition to the risks common to all surgery and the risks associated with anesthesia, there are a few risks more specific to this surgery:
A hematoma may develop in your knee following the procedure and require further arthroscopic lavage.
Phlebitis can occur whether or not you are on anticoagulant treatment. This results in pain in the calf. Diagnosis and treatment must be carried out quickly for recovery in a few weeks, generally without sequelae.
Algodystrophy resulting in painful stiffness. Diagnosis is made by bone scan and treatment includes calcium injections.
Anterior cutaneous hypoesthesia which results in a change in the sensitivity of the anterior surface of your knee (impression cottony to the touch). This phenomenon is generally resolved after a few months.
Exceptional chondrolysis may occur during the treatment of certain external meniscal lesions. A stroll with English canes is then justified until the knee dries up.
The occurrence of a painful popliteal cyst remains exceptional. The symptoms gradually disappear over time. Some cysts may persist and become bothersome; in this case their surgical excision is desirable.
The risks listed above are rare but do not constitute an exhaustive list. Your surgeon will give any additional explanation and will be at your disposal to discuss with you each particular case with the advantages, disadvantages and risks of the intervention.