Total hip prosthesis (THA)
What is?
The worn or damaged hip joint is operated on and the joint surfaces are replaced with an artificial joint called a joint prosthesis (total hip prosthesis).
What is a joint?
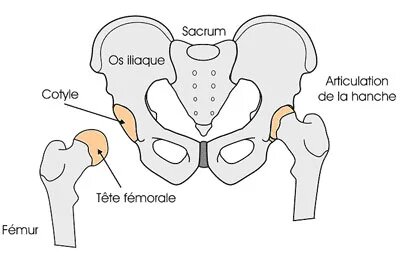 A joint is formed by the ends of two or more bones that are attached together by ligaments and the joint capsule . Your hip joint is formed by the femoral head and the part of the pelvic bone that receives it called the acetabulum or acetabulum. This acetabulum is an integral part of the iliac bone.
A joint is formed by the ends of two or more bones that are attached together by ligaments and the joint capsule . Your hip joint is formed by the femoral head and the part of the pelvic bone that receives it called the acetabulum or acetabulum. This acetabulum is an integral part of the iliac bone.
The bone ends in contact are covered with a layer of cartilage. Normal cartilage allows movement without pain and without resistance. When cartilage is damaged by osteoarthritis or other joint diseases, joints become stiff and painful.
Each joint is surrounded by an envelope of fibrous tissue, the capsule, reinforced by ligaments and covered on the inside with a very thin membrane: the synovium.
The synovial membrane produces fluid that reduces friction and wear and tear on the joint. When produced in excess, it is "synovial effusion".
Why is it necessary to replace this articulation?
The aim is to eliminate pain caused by wear or deterioration of articular cartilage, restore mobility and correct deformities at least partially. The pain can be so great that the subject will use his joint less and make it more difficult to move the joint, hence the discomfort in daily life: walking, stairs, washing, foot care, dressing, etc... sometimes reduced autonomy.
The clinical examination, some laboratory tests, and x-rays will show the intensity of the wear of the cartilage, its alteration and deformations. The replacement of the joint (arthroplasty) by a prosthesis will be considered when other conservative treatments do not eliminate your pain and your disability.
Classically, a hip prosthesis eliminates pain, and restores mobility and normal walking distance (total distance the patient can cover without stopping).
How do we do it?
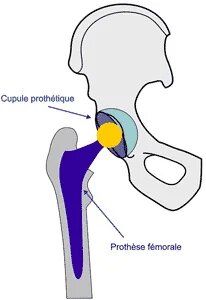 The surgeon replaces the damaged cartilaginous and bony parts of the joint.
The surgeon replaces the damaged cartilaginous and bony parts of the joint.
The damaged femoral head is replaced by a femoral prosthesis (stem) placed in the femur as a "pivot", and a prosthetic cup is implanted in the iliac bone to replace the damaged acetabulum with, in between, friction torque for mobility.
Your hip joint is formed by the femoral head and the part of the pelvic bone that receives it called the acetabulum or acetabulum. This acetabulum is an integral part of the iliac bone.
While hip and knee prostheses are the most common interventions, joint replacement can be performed in other joints, ankle, shoulder, elbow … etc.
The materials used are designed to restore movement to the joint as close as possible to its mechanics normal.
The prosthesis has a friction couple: a metal or ceramic part slides into a material part plastic or other, metallic or ceramic.
Several metallic materials are used, chromium and cobalt alloy, titanium, stainless steel; they can be coated (hydroxyapatite) to improve fixation to bone.
The plastic material is resistant (very high density polyethylene). Friction can be done with alumina ceramic, metal.
An acrylic cement (polymethyl - methacrylate) can be used to improve the initial fixation of the prosthesis in the bone, ("like at the dentist"). Articular prostheses can also be implanted without cement, if the shape of the prosthesis and of the bone allow satisfactory adaptation and mechanical resistance from the outset.
The size of the skin incision (scar) depends on different parameters (height-weight morphotype , initial hip disease, deformation, risk of fracture). The "mini incisions" do not only have advantages, large scars are not mandatory.
How is rehabilitation going?
You will probably have met your physiotherapist before the procedure, either during the anesthesia consultation or the day before your procedure. Typically, your orthopedic surgeon will encourage you to use your new joint soon after your operation. After a total hip prosthesis, you will be up and walking the day after the procedure with assistance. At first, you will walk with a walker, then English canes until you simply forget.
Most patients have temporary postoperative pain in the operated joint during the recovery phase. tissue healing. Analgesia is administered effectively (opioids, etc.). The pain will be relieved immediately after the operation. It will subside spontaneously and gradually after a few days. Exercises are an important part of the rehabilitation procedure. The physiotherapist will begin his care the day after the intervention. Exercises will be requested and taught. Rehabilitation will then continue either externally, at home then in the office of a physiotherapist, or in a convalescent center where you will be hospitalized for 2 to 3 weeks following hospitalization at the Hospital, all this depending on your personal organization and the initial illness
The mobility of your operated joint will gradually increase after the procedure. The quality of the movement obtained depends most of the time on preoperative stiffness, hence the need for its maintenance preoperatively. Control consultations will be carried out at 3 months, 6 months, 1 year and then every 2 years or 5 years depending on the initial and secondary circumstances.
Preparing for arthroplasty
Before the intervention, your surgeon and your anesthetist will recommend that you stop taking certain medications (ASPIRINE and anti-platelet aggregates) for fifteen days before the intervention, to contact the Blood Transfusion Center to carry out, if necessary possible (before the age of 75), samples of your own blood to avoid having to resort to a transfusion after the intervention (programmed auto-transfusion), starting exercises (exercise bike) before the intervention to accelerate the postoperative recovery, finally, to assess the practical possibilities for rehabilitation, depending on your place and your way of life (organization of the house, entourage, etc.) and for the resumption of autonomy (raised toilet, shower, clamp prehensive…).
Is your joint prosthesis permanent?
Older people can hope that their joint prosthesis will accompany them for the rest of their lives. This will provide them with years of pain-free life, which otherwise would not have been possible.
Younger patients may require a second procedure due to natural wear of the prosthesis , this is likely if you are under 50 at implantation. This justifies follow-up consultations, initially annually then more spaced out, to watch for abnormal bone remodeling in contact with the implants, before the pain appears again and is associated with a loss of bone capital that can go as far as loosening and to monitor wear.
The efforts of surgeons and engineers in the field of surgical techniques and biomaterials give hope for the future a greater longevity of the implants. 5% of currently implanted prostheses are operated on again in the next 15 to 20 years. The others (95%) will not be operated on again within these timeframes and 90% give satisfaction at 20 years.
The future remains bright for those who choose to have a joint prosthesis, because it improves the quality of life, allows them to acquire greater independence and to regain activity without pain, a guarantee of good health. It typically allows them to walk without pain, without limping as long as they want.
What are the possible complications?
A Inform your orthopedic surgeon and the anesthesiologist of any pathology you are carrying or any illness that could influence the operation. Articular prosthetic surgery gives excellent functional results in more than 90% of cases. When complications do occur, most are controlled and treatable. It is estimated that 5% of prostheses are re-operated for insufficient results within 15 years of their implantation.
Fractures of the pelvis or femur. They can occur during implantation because the components are implanted in force if they are not sealed. They sometimes require fixation and can delay full support for a few weeks (3 to 5). Sealing is not a guarantee of absence of intraoperative fracture. They are often related to bone quality.
Phlebitis. Phlebitis results from several factors, the main one being the decrease in mobility observed during and after the operation. The treatment of varicose veins as a preventive measure may sometimes be necessary. A preventive treatment is systematically applied, with subcutaneous injections of anticoagulants from the intervention. This preventive treatment should last approximately one month to 45 days. Wearing compression stockings is necessary to also reduce the risk of phlebitis and to get up early (the next day). Despite all these preventive measures, however, phlebitis can occur. Its early diagnosis and treatment are the factors for rapid recovery. It can lead to pulmonary embolism, which is a serious but rare complication. The diagnosis must be made early in front of pain in the calf, to be treated effectively with anticoagulants.
Ossifications. They cause stiffness if they are significant, which is rare. They usually do not change the result. They may justify irradiation at anti-inflammatory doses (radiotherapy).
Unsealing. The loosening of a prosthesis can occur following an arthroplasty. This is the cause of the resumption of pain when walking. It is related to the reaction to wear products. A reoperation is necessary. Modern fixation methods and improved friction torques of prostheses should reduce the risk of long-term loosening (5% at 15 and 20 years), but loosening can indicate infection (see below).
Dislocations. Sometimes, after a total hip prosthesis, the femoral head can "dislocate". In most cases, the hip can be put back in place without resorting to a new procedure. Most often, dislocations occur when the muscle condition is failing, or when it is a reoperation. The physiotherapist will teach you the movements to avoid to reduce the risk of dislocation according to the surgical technique used in the initial period, the most frequent period of occurrence. Late dislocations, on the other hand, are signs of wear and tear on the friction couple.
Wear. Some degree of wear and tear is natural in any artificial joint over time due to friction. Excessive wear can lead to loosening or late dislocations and may require prosthetic revision surgery.
Rupture or mechanical failure of implants. Rupture of a metal, polyethylene or ceramic implant is very rare, but it can occur. A new intervention is necessary in these cases. Femoral stem ruptures are observed when there is no bone in contact with the femoral prosthesis even though the latter is well fixed at its distal end. These are stress fractures. The implants are subject to resistance standards but rupture can always occur. It is evaluated at approximately 1 in 10,000 for ceramic friction.
Nerve trauma. The nerves in the vicinity of the joint prosthesis can be damaged. This type of complication is very rare. It can occur especially when the intervention must correct a major deformation of the joint, or a significant shortening of the lower limb. Most of the time, these nerve injuries will recover, but more or less completely within a few months.
The length inequality. It is exceptionally disabling with a compensating heel piece. It rarely exceeds 1cm to 1.5cm (depending on the size of the patient). Shortening without a heel pad is better tolerated than lengthening. It depends on the morphological conditions of the hip.
The infection on prosthesis.
What is the treatment for an infected prosthesis?
The superficial infection evolves favorably with an antibiotic treatment which is not always obligatory.
The deep infection justifies a real treatment, with most often the need for a reoperation, the removal of the prosthesis linked to the adhesion phenomenon, replanting, either immediately or secondarily (a few weeks to several months), depending on the time of onset of the infection, the bacteria detected, the sensitivity to antibiotics, data from biological examinations, etc. Antibiotic treatment is regularly intravenously for a few weeks and then by mouth (per os) for several months. During the period without a prosthesis, the patient walks with two canes. Such a strategy makes it possible to find the use of the articular prosthesis with a functional quality close to that obtained regularly from the outset.