Endoscopic urethrotomy
Defintion
 Internal urethrotomy consists of the endoscopic treatment of the narrowing of the urethral canal of different etiology. The objective is to incise and open the narrowed urethral canal in the hope that this increase in caliber will be maintained over time.
Internal urethrotomy consists of the endoscopic treatment of the narrowing of the urethral canal of different etiology. The objective is to incise and open the narrowed urethral canal in the hope that this increase in caliber will be maintained over time.
Indications
Congenital (urethral valves) and acquired strictures of the urethra.
Intervention
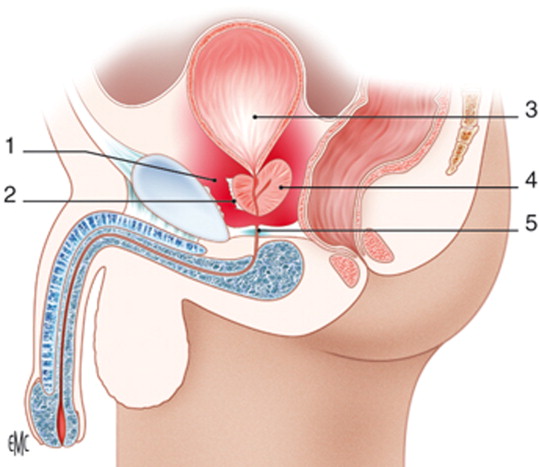
Endoscopic incision of the urethral canal with a “cold” blade can be performed blind (Otis urethrotomy) or under vision (Sachse urethrotomy).
The surgery usually lasts a few minutes and can be performed under general and loco-regional anesthesia. Sometimes a simple sedation of the patient may also be sufficient.
Recovery
A bladder catheter is left in place after surgery. In the absence of complications, the duration of hospitalization is 1 to 2 days.
Temporary bleeding between the catheter and the urethral meatus may occur in the immediate postoperative period.
Results
After catheter removal, there is a disappearance of obstructive symptoms with an improvement in voiding parameters. In anterior urethral strictures (penile and bulbar), the long-term positive results of internal urethrotomy (30%) are significantly lower than those of open urethroplasty surgery (90%).
In stenosis of the posterior urethra (membranous and prostatic) internal urethrotomy gives better results than in the anterior urethral tract but still inferior to open surgery.
Advantages
Less invasive than open surgery (urethroplasty).
The only treatment possible in certain cases where urethroplasty would risk compromising erection or urinary continence.
No high fees.
Low complication rate.
Disadvantages
Low long-term success rate.
Histologic examination not performed.
Urethral wall involvement following endoscopic surgery can transform a short, simple urethral injury into a longer and more complicated lesion requiring more complex surgical repair than before endoscopic treatment: this represents the major drawback of internal urethrotomy.
Complications
Perforation of the urethral wall (false passage) can lead to the formation of urethral fistulas and periurethral abscesses.
Postoperative
Urinary antiseptic treatment until the third day following removal of the bladder catheter.
In patients with a urethral scar lesion potentially at risk of fibro-sclerotic evolution with recurrence of the stenosis, it is recommended to avoid any possible traumatic action on the genito-perineal region in the months following the intervention: avoid the use of cycles, motorcycles, tractors, horses; avoid prolonged sitting, especially on rigid seats; avoid contact sports which can cause trauma to the affected area; respect dietary rules (avoid white wines, sparkling wines, beer, spicy foods).
During the months following the urethrotomy, the patient must carry out periodic checks to assess the validity of the urinary output and bladder emptying: uroflowmetry and bladder ultrasound.
If, on the basis of these tests, there is doubt about a recurrence of the urethral stricture, the urologist may decide to deepen the investigation with retrograde and voiding urethrography and urethroscopy.