Artificial Insemination Technique
Definition
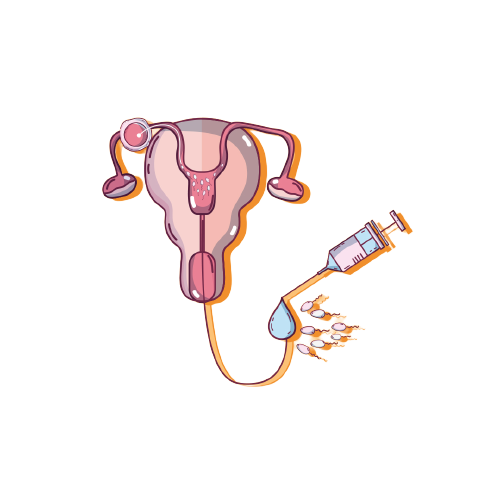 Artificial insemination is a medically assisted reproduction technique used in the treatment of infertility.
Artificial insemination is a medically assisted reproduction technique used in the treatment of infertility.
Basically, the method provides for the introduction of the male semen, artificially, into the female reproductive system.
Artificial insemination is performed during the periovulatory period on a spontaneous cycle or after moderate pharmacological stimulation. The goal is to promote the spontaneous meeting of the two gametes (female oocytes and male sperm) in the female body.
The chances of becoming pregnant vary from 10% to 15% per attempt, depending on the underlying disease and the age of the patient.
Artificial insemination is a first-level medically assisted procreation technique (PMA). This method is therefore one of the simplest and least invasive therapeutic options recommended for a couple who wish to have a child, but who cannot become pregnant spontaneously.
Artificial insemination techniques
The methods of carrying out artificial insemination differ according to the site where the semen is deposited:
Intrauterine insemination (IUI): the most commonly used technique, in which sperm are introduced directly into the uterus;
Intracervical insemination (ICI): Sperm are introduced into the cervical canal. This method is preferred when there is no possibility of semen depositing in the vaginal fornices.
Intraperitoneal insemination (IPI): consists of the inoculation of seminal fluid into the cavity of Douglas (between the rectum and the posterior wall of the uterus). This technique is little used, because it predisposes more to the development of anti-sperm antibodies.
Tube insemination (ITI): it is performed if the woman's tube is in perfect condition and when other techniques have failed. Thanks to a catheter and under the constant guidance of ultrasound, the seminal fluid is introduced into the fallopian tubes, the natural meeting place between spermatozoa and oocytes.
Depending on the partner, artificial insemination can be divided into:
Conjugal artificial insemination (ACI) or homologous: involves the use of homologous gametes, i.e. say from the components of the couple. This procedure can be useful in cases of slightly reduced male fertility (total sperm concentration or highly motile sperm count slightly lower than normal) and in the absence of tubal occlusion in women.
Artificial insemination from a donor (AID) or heterologous: involves the use of sperm from a a sperm bank; this method is suitable when the characteristics of the seminal fluid are such that they completely compromise reproductive functionality.
When is artificial insemination indicated?
Artificial insemination is considered when targeted intercourse (ie during days of probable ovulation) and/or drug ovarian stimulation are associated with repeated failures.
Artificial insemination is indicated in case of:
Infertility of unknown origin (i.e. to which a precise cause cannot be attributed ).
Cervical or tubal factors (anatomical and/or functional alterations of the cervix, cervical mucus or one or both fallopian tubes).
Slight to moderate alterations in certain seminal fluid parameters, such as sperm have difficulty reaching the uterus.
Coital difficulties or hindrances to the sexual act (as, for example, in the case where the woman suffers vaginismus or the male partner has had a vasectomy or has recurrent episodes of impotence).
Artificial insemination can compensate for abnormalities in male sperm because sample preparation before the procedure helps separate viable, motile sperm from lower quality ones.
Artificial insemination can also be used if the male partner suffers from:
Retrograde ejaculations (in the bladder) caused by prostate surgery.
Certain pathologies of the genital tract, such as hypospadias, in which it is difficult or impossible to to have full sex.
With regard to women, however, artificial insemination is indicated in the presence of:
Mild endometriosis.
Ovulatory dysfunctions.
Immunological factors (eg, development of anti-sperm antibodies)
Exigences
As part of the treatment of infertility, before embarking on this process, the doctor checks that the following conditions exist:
Tubal patency.
Absence of infections in the male and female genital tract.
Quality (movement and morphology) and acceptable sperm count.
Indeed, for the success of artificial insemination, it is essential that the oligo-asthenospermia is mild or moderate and that the tubal function is preserved (at least unilaterally).
How is it going?
Artificial insemination is a medically assisted procreation technique that respects the normal stages of the reproductive process. The technique is ambulatory, minimally invasive and painless.
Ovulation stimulation
Artificial insemination can be implemented on a spontaneous cycle or with stimulation of ovulation by the administration of drugs (usually recombinant gonadotropins), from the second or third day of the start of the menstrual cycle.The goal is to induce the ovaries to produce more than one follicle and to obtain the simultaneous maturation of 2-3 eggs, to increase the chances that at least one of them will be fertilized.Ultrasound monitoring of ovulation, carried out during treatment, makes it possible to modify the dose of drugs to optimize the ovarian response.Based on the size of the follicles and the thickness of the uterine lining, it is possible to predict the time of ovulation in the current cycle.Usually, as soon as two or three follicles have reached a certain size (about 18 mm), ovulation is induced by injection of human chorionic gonadotropin (hCG), so that the most suitable time can be used for insemination .
Semen preparation
The sperm necessary for artificial insemination is obtained by masturbation after 2 to 5 days of abstinence (in order to increase the level of sperm) or by puncture of the vas deferens.The sample thus obtained undergoes a special preparation in the laboratory, ie it is treated in such a way as to select and concentrate the motile spermatozoa in a sufficient volume.
Insemination
The day of artificial insemination is fixed 36 hours after the administration of hCG. The seminal fluid of the partner or a donor, previously examined and subjected to selection, is released into the reproductive system of the patient (according to the method: uterine cavity, cervical canal or fallopian tube), via a fine catheter.It is a simple, painless process and very similar to any gynecological visit.14 days after insemination, plasma β-hCG assay will be performed, to check if a successful pregnancy has been established.
Success rate
Artificial insemination is associated with good results. The chances of getting pregnant with this technique are 10-15% per treatment cycle.
The success rates of this technique vary depending on:
Causes of infertility present in the couple.
The age of the patient.
Qualitative and quantitative characteristics of seminal fluid.
Type of pharmacological stimulation performed.
Generally, if conception does not occur after 3-4 cycles of artificial insemination, it is advisable to reassess the case and move on to another more sophisticated procedure, such as in vitro fertilization.